Your client is here.
You, at a normal pace, hurry to greet them but quickly slow in approach as you watch them rise from their seat with the movement quality of someone 50 years their senior.
The slow rise finishes with qualities of an old machine attempting to shift into a locked position as they intensely brace themselves through the maximal slow strenuous effort to extend their hips and spine to an upright posture.
You start your steps toward the treatment room but by your second step you realize you already passed your client 6 feet ago. You realize, it’s time to be here now.
The journey to your treatment room provides time to review testing findings and discussions both you and the client’s had coordinated with other disciplines. The patients words require significant effort for them to express.
Their words have a defeated and tired air to them but they certainly are giving all their effort.
The travels, the demands of work and the significant struggles in family life, the sheer tenacity and will to keep going in spite of a body that screams for rest. Life must go on after all does it not?
You observe the posturing that looks that of a much frailer representation of the younger client who stand before you. Your mind wants to speak of the antalgic changes in kinetic loading from foot to head and the way the sandals are worn on the feet to allow for some relief but now is not the time. The rigid shoulder and arm posturing, the clenching of the fists, and the strain of the words coming from their mouth.
You arrive at your treatment room, you lower the table. Already all plans for the session have changed four times since you first greeted your client.
Every plan shift reviewed systems, symptoms, behavior, client report, reconsideration of other discipline objectives, the social and work constraints presented by the client. Where is my entry point today, no not there, ah there, no the time is not right, could they progress on that from before, are they ready for this? No not now, let them lead.
You place the chair but the client opts for the table. They do not know their body, they do not know the struggle they themselves are adding the problem, but words do not matter now. Only the bolster and hands on guidance for ease.
The client exhales a sigh of relief for a moment, their eyes change as they seem to indicate that they just learned something in that process, and they thank you for helping them.
You notice the swelling of both ankles are improved since the last session and the client reports they are seeing improvements since the first session with the strategies you had discussed.
You know the relief is short lived and begin planning in the background the next steps and how those steps could be used to further educate and empower the patient to learn know their own needs better. You balance your words in your mind as you find ways to both the dance with the complexity of, dare I label and define it?
Moments later the next wave has arrived and stuns the client into a heightened state once again. They steel themselves and demonstrate an intensive muscular effort of the back and hips that they report provides them momentary relief of both legs but worsens their back.
The session now reveals itself dynamically.
The dance of the dialog and interactions of session now reaches a flow point. You and your client work together to engage the suffering and workability of their struggle with pain.
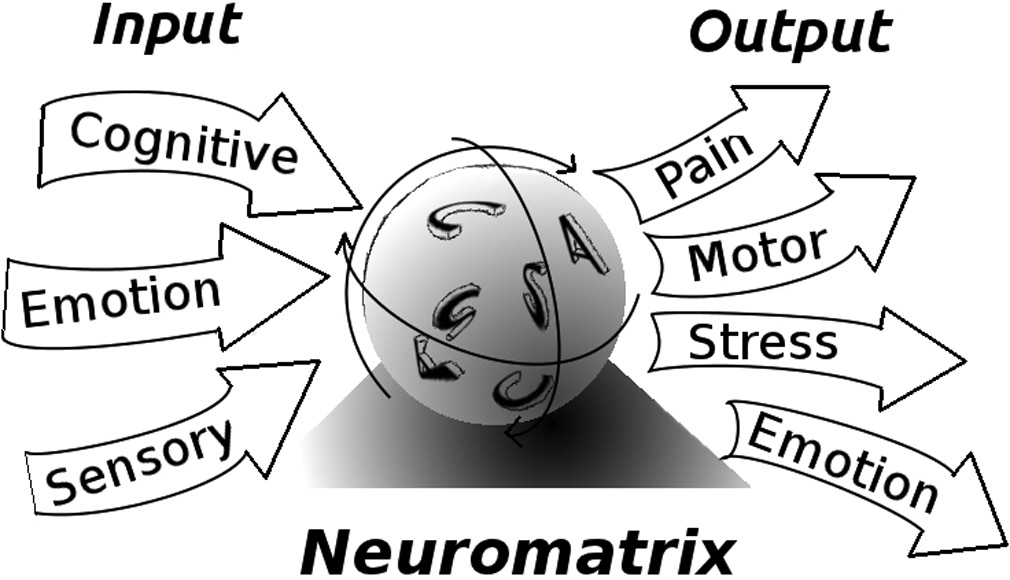
The dance is certainly technical, from review and progressing of meaningful understanding and application of the physiology, the cognitive, the emotion, and the social interactions.. To managing the biomechanical outputs through hands on guidance and coaching of positioning relief to allow them to appreciate value of awareness and exploration of the automatic postural and guarding response of the human body. The larger picture unfolds and the conversation naturally leads to where the client is going to engage in the process. The artistic beauty of the interaction paints the picture, rather than the technical details.
The client breaths comfortably. The pain is less, but this not important. What is important is that the meaning of the pain has changed. They feel hopeful and they know their role in the process going forward.
The time allotted is now over. Now the journey from the sterility, but subtle safety, of the room to the clients own reality begins. They arise now taller, there is a lightness present in their movement, and there is strength in their words.